RANIBIZUMAB, solution for intravitreal injection, 2.3 mg in 0.23 mL, Lucentis®, Novartis Pharmaceuticals Australia Pty Ltd
PDF printable version of this page
1 Purpose of Application
1.1 A minor resubmission for the treatment of visual impairment due to diabetic macular oedema (DME) and macular oedema secondary to retinal vein occlusion (RVO), to address concerns raised by the November 2013 PBAC meeting.
2 Requested listing
2.1 The requested listing was unchanged from that requested in November 2013.
2.2 As previously, listing was sought on the basis of superior comparative effectiveness and equivalent comparative safety compared with laser photocoagulation (DME and branch RVO) and best supportive care with observation (RVO).
3 Background
3.1 Ranibizumab was TGA registered 5 August 2011 for the treatment of visual impairment due to DME and 30 November 2011 for the treatment of visual impairment due to macular oedema secondary to RVO.
3.2 Ranibizumab has been PBS-listed for the treatment of wet age-related macular degeneration (wAMD) since August 2007. The PBAC considered ranibizumab for the treatment of visual impairment due to DME in March 2013, and for treatment of macular oedema secondary to RVO in November 2012. Both of these submissions were rejected, and resubmissions were considered at the November 2013 PBAC meeting.
3.3 At its November 2013 meeting, the PBAC deferred its consideration of ranibizumab for DME and RVO. The minor resubmission “seeks to address concerns raised by the PBAC that the unregistered and unlicensed use of bevacizumab means it is a relevant comparator for ranibizumab in DME and RVO” (pg 3 of minor resubmission).
3.4 At its November 2013 meeting, the PBAC considered it was important to resolve the issue of whether bevacizumab can be used as an appropriate comparator for ranibizumab, and if so, how a clinical and economic comparison versus bevacizumab could be conducted, and any implications of conducting such a comparison given bevacizumab is neither PBS-listed not TGA approved for the diabetic macular oedema (DME) and RVO indications.
4 Clinical place for the proposed therapy
Diabetic macular oedema (DME)
4.1 DME is a complication of diabetic retinopathy. It is diagnosed by ophthalmic examination, fluorescein angiography and fundus photography. When DME affects the centre of the macula, it can lead to loss of visual acuity, and if left untreated, to blindness. The natural progression of DME leads to a significant loss (?10 letters) within two years in 50% of individuals.
Retinal vein occlusion (RVO)
4.2 RVO is a blockage of the vessel which drains blood out of the retina, the light-sensitive tissue at the back of the eye. The blockage results in increased pressure within the blood vessel causing blood and fluid to leak from the blood vessels into the retina. This can result in swelling or thickening of the retina (oedema). Occlusions are categorised into branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO) based on the site of the occlusion.
5 Comparator
5.1 The PBAC considered that laser photocoagulation (DME and branch RVO) and best supportive care with observation (RVO) in the absence of injected therapy were relevant comparators and that the submitted sham-controlled trials provided relevant information for PBAC to compare ranibizumab with best supportive care.
5.2 The PBAC considered that compounded bevacizumab was also a relevant comparator because evidence of its current use in patients who would be eligible for PBS-subsidised ranibizumab means that prescribers would replace compounded bevacizumab in practice with ranibizumab if the PBS subsidises ranibizumab.
5.3 The PBAC noted the applicant's arguments against accepting bevacizumab as a comparator, principally on the grounds that this represents use beyond the TGA-approved indications and adapting a formulation which is not intended for injection into the eye. However, the PBAC noted that Subsection A.4 of the PBAC Guidelines states that "PBAC bases its judgement about the main comparator on what would be likely to happen, rather than what should happen, in keeping with the above definition of the main comparator." The PBAC noted that an evidence base beyond the sham-controlled trials was needed to assess the comparison of compounded bevacizumab with ranibizumab.
5.4 The PBAC noted Departmental advice that, if compounded bevacizumab were to be considered for PBS listing, its pricing for PBS purposes would most likely reflect the approach to pricing already applied to bevacizumab as an oncology medicine through the Efficient Chemotherapy Funding Program.
6 PBAC consideration of the evidence
6.1 The PBAC noted and welcomed the input from individuals (3), health care professionals (2) and organisations (6) via the Consumer Comments facility on the PBS website. The comments described a range of benefits of treatment with ranibizumab including:
- better eyesight
- reduction in financial burden
- improvement to quality of life.
6.2 The PBAC noted the support for listing from Diabetes Australia, Vision 2020 Australia, Royal Australian and New Zealand College of Ophthalmologists, Macular Disease Foundation of Australia and the Australia Diabetes Council.
Clinical trials
6.3 The minor resubmission stated that clinical efficacy of ranibizumab has been presented previously to the PBAC in the RESTORE and DRCR.net trials for diabetic macular oedema (DME) as well as the BRAVO and CRUISE trials for retinal vein occlusion (RVO). For DME, the November 2013 PBAC Minutes (paragraph 6.15) indicate that the PBAC recalled that it had previously considered that, in a single treated eye in each patient, ranibizumab is probably superior to laser photocoagulation if it is accepted that a difference of 5 letters is clinically important. For RVO, the November 2013 PBAC Minutes (paragraph 6.11) indicate that the PBAC agreed with the claim that ranibizumab has superior effectiveness over laser treatment for BRVO and superior effectiveness over observation for CRVO, but did not agree with the claim for similar safety.
6.4 The minor resubmission presented one head-to-head trial comparing ranibizumab and bevacizumab in DME (Nepomuceno et al., 2013) and no head-to-head RVO trials. Consequently, the RVO evidence presented in the minor resubmission focused on evidence available in four systematic reviews (Anothaisintawee 2012; Mitry 2013; Pielen 2013; Van der Reis 2011). The Anothaisintawee 2012 review provided an indirect comparison of ranibizumab and bevacizumab for both BRVO and CRVO combined. Because the previous RVO resubmissions have presented evidence for BRVO and CRVO separately, the minor resubmission selected available evidence from the three remaining reviews comparing bevacizumab and sham injection in CRVO and bevacizumab and laser/sham injection in BRVO. The table below provides a summary of the clinical evidence presented in the resubmission.
|
Trial |
N |
Design/ duration |
Patient population |
Risk of bias |
Comparison/ outcome |
|---|---|---|---|---|---|
|
DME – ranibizumab vs. bevacizumab |
|||||
|
Nepomuceno 2013 |
48 |
R, DMa |
center-involved DME, central subfield thickness >300 mm; BCVA 20/40 to 20/800 |
Unclear |
Ranibizumab vs. bevacizumab Change in BCVA, CSMT |
|
RVO – indirect comparison sourced from Anothaisintawee 2012 systematic review |
|||||
|
Anothaisintawee 2012 |
899 |
SR |
|
||
|
CRUISE |
362 |
R, DM, MC |
CRVO, mean retinal thickness ?250?m; BCVA of 20/40 to 20/320 |
Low |
Ranibizumab vs. sham injection; mean change in BCVA at week 24 |
|
BRAVO |
397 |
R, DM, MC |
BRVO; BCVA 20/40 to 20/400; mean CST ?250?m |
Low |
Ranibizumab vs. laser/sham; change from baseline in BCVA at 6 months |
|
ROCC |
29 |
R, DM, MC |
CRVO |
Low |
Ranibizumab vs. sham injection; BCVA and CMT at 6mths |
|
Moradian 2011 |
81 |
R, DM |
Acute BRVO and BCVA ?20/50 |
Low |
Bevacizumab vs. sham injection; change in BCVA and CMT at 6 and 12 weeks |
|
CRVO direct evidence (no indirect comparison undertaken) |
|||||
|
CRUISE |
As above |
||||
|
Epstein 2012 |
60 |
R, DM |
CRVO, mean retinal thickness ?300?m; BCVA of 20/50 to 20/500 |
Low |
Bevacizumab vs. sham injection; proportion of patients gaining ?15 EDTRS letters at 6 months |
|
Faghihi 2008 |
101 |
No information available |
|||
|
BRVO direct evidence (no indirect comparison undertaken) |
|||||
|
BRAVO |
As above |
||||
|
Russo 2009 |
30 |
OL |
Perfused BRVO |
High |
Bevacizumab vs. laser; change in BCVA logMARb |
|
Moradian 2011 |
81 |
R, DM |
Acute BRVO and BCVA ?20/50 |
Low |
Bevacizumab vs. sham injection; change in BCVA and CMT at 6 and 12 weeks |
a The clinicaltrials.gov listing for this trial states that it is an open-label trial; the published paper states that it is double-masked.
b BCVA logMAR refers to best corrected visual acuity (BCVA) determined from the Early Treatment Diabetic Retinopathy Study (ETDRS) chart and calculated as logarithm of minimal angle resolution (logMAR).
CMT=central macular thickness; CSMT=central subfield macular thickness; DM=double-masked; MC=multi-centre; OL=open label; R=randomised; SR=systematic review
Source: compiled during the evaluation
6.5 The minor resubmission did not provide any information regarding the outcomes assessed or the statistical methods used in the included trials. When describing trial and review results, the minor resubmission uses general terminology such as ‘bevacizumab and ranibizumab were equally efficacious’.
6.6 The PBAC noted that there are currently many relevant trials either ongoing, or expected to begin enrolling in the near future. These trials are listed in the table below.
|
Trial |
Comparison |
Design |
Completion date |
Status |
|---|---|---|---|---|
|
RVO trials for bevacizumab (ongoing and future) |
||||
|
NCT01635803 |
Trial comparing costs and effectiveness of bevacizumab and ranibizumab for RVO |
R, DM |
Not provided (estimated primary completion date is June 2016) |
Still recruiting |
|
NCT01428388 (CRAVE) |
Bevacizumab vs. ranibizumab for macular oedema secondary to RVO |
R, SM |
January 2014 (estimated) |
No data available |
|
NCT01969708 |
Non-inferiority trial comparing bevacizumab and aflibercept for the treatment of macular oedema secondary to CRVO |
R, SM |
Not provided (estimated primary completion date is March 2018) |
Trial not yet commenced. |
|
*NCT01918371 |
Retrospective study comparing bevacizumab, ranibizumab and aflibercept in patients with RVO and DME |
O |
June 2014 (estimated) |
No data available |
|
NCT00906685 |
Trial comparing efficacy of bevacizumab with sham injection in CRVO |
R, DM |
Completed |
No data available |
|
DME trials for bevacizumab |
||||
|
NCT01635790 (BRDME) |
Trial comparing costs and effectiveness of bevacizumab and ranibizumab for DME |
R, DM |
Not provided (estimated primary completion date is June 2016) |
No data available |
|
NCT 01627249 |
Comparative effectiveness of bevacizumab, ranibizumab and aflibercept for DME |
R, SM |
September 2015 |
No data available |
|
NCT01610557 (CADME) |
Phase 2 trial comparing bevacizumab and ranibizumab for DME |
R, DM |
August 2014 (estimated) |
No data available |
|
NCT01487629 (IBERADME) |
Comparative efficacy trial of bevacizumab and ranibizumab in DME |
R, OL |
September 2012 (unverified) |
No data available, recruitment status unverified by clinicaltrials.gov |
BRDME=Comparing the Effectiveness and Costs of Bevacizumab to Ranibizumab in Patients With Diabetic Macular Edema; CADME=A Phase II Randomized Study to Compare Anti-VEGF Agents in the Treatment of Diabetic Macular Edema; DME=diabetic macular oedema; IBERADME=Bevacizumab Versus Ranibizumab for the Treatment of Diabetic Macular Edema; ME=macular (o)edema; O=observational; OL=open label; R=randomised; RVO=retinal vein occlusion; SM=single masked.
*This study is a retrospective observational study. It has been included due to larger sample size and its comparison of all three anti-VEGF agents.
Comparative effectiveness
Diabetic macular oedema (DME)
6.7 The minor resubmission stated that the Nepomuceno 2013 trial demonstrated that bevacizumab and ranibizumab were equally efficacious, but not at an equal number of injections (mean injection number being 9.48 for bevacizumab and 7.67 for ranibizumab). The minor resubmission does not provide any numerical results to support the claim of ‘equally efficacious’. The Nepomuceno 2013 publication provides mean BCVA at each follow-up point and a corresponding P-value for the comparison between bevacizumab and ranibizumab. These results are provided in the table below. There was no statistically significant difference between the two treatment groups at most time points, with the exception of weeks 8 and 32, when ranibizumab had a statistically higher mean BCVA than bevacizumab. The mean number of injections claimed by the minor resubmission are the number of injections at week 48, with the difference in injections being statistically significant (p=0.005). Interpretation of these results should take into consideration the small size of the trial (N=48 patients; 63 eyes) and the potential for risk of bias given that almost a quarter of study eyes (24%) were not randomly allocated. In addition, although the published article states that examiners, outcomes assessors, OCT technicians, fundus photographers and patients were masked, the page for this trial on clinicaltrials.gov states that the trial is open label. This evidence on its own is insufficient to inform an assessment of non-inferiority.
|
Week |
Bevacizumab (N=32 eyes) Mean BCVA logMAR (SE) |
Ranibizumab (N=28 eyes) Mean BCVA logMAR (SE) |
p value |
|---|---|---|---|
|
0 |
0.6 (0.05) |
0.63 (0.06) |
- |
|
4 |
0.48 (0.06) |
0.53 (0.06) |
0.66 |
|
8 |
0.48 (0.06) |
0.46 (0.06) |
0.03 |
|
12 |
0.45 (0.05) |
0.46 (0.05) |
0.19 |
|
16 |
0.42 (0.05) |
0.43 (0.06) |
0.25 |
|
20 |
0.41 (0.05) |
0.42 (0.06) |
0.26 |
|
24 |
0.41 (0.05) |
0.4 (0.05) |
0.15 |
|
28 |
0.43 (0.06) |
0.4 (0.05) |
0.07 |
|
32 |
0.41 (0.06) |
0.36 (0.04) |
0.04 |
|
36 |
0.4 (0.06) |
0.36 (0.04) |
0.05 |
|
40 |
0.39 (0.06) |
0.35 (0.04) |
0.06 |
|
44 |
0.36 (0.05) |
0.34 (0.04) |
0.13 |
|
48 |
0.36 (0.05) |
0.34 (0.04) |
0.19 |
Source: Nepomuceno et al 2013 Table 2 p. 505
BCVA=best corrected visual acuity; logMAR=logarithm of minimum angle resolution
Retinal vein occlusion (RVO)
6.8 The minor resubmission reported results from the systematic review of Anothaisintawee 2012, which provided an indirect comparison of ranibizumab and bevacizumab for BRVO and CRVO combined. The minor resubmission reported no significant difference in visual acuity outcomes with a MD=3.39 (95% CI: -10.55, 17.33) and no difference in serious adverse events with RR=1.14 (95% CI: 0.39, 2.65). For mean change in visual acuity, the indirect comparison in the Anothaisintawee 2012 systematic review used 3 trials comparing ranibizumab and sham injection/laser in CRVO (CRUISE) and BRVO (BRAVO, ROCC) and 1 trial comparing bevacizumab and sham injection in BRVO (Moradian 2011). Therefore, the indirect comparison may be biased as it compares CRVO and BRVO trials with a much smaller BRVO trial. In addition, the results presented in the Anothaisintawee 2012 review could not be verified as minimal data was presented in the review.
6.9 The minor resubmission stated that since the PBAC submission presented ranibizumab data independently for CRVO and BRVO, a review of the bevacizumab evidence for CRVO and BRVO, that includes the same comparator as in the CRUISE and BRAVO trials, will be presented. The minor resubmission did not present a review of such evidence.
6.10 The minor resubmission stated that the six CRVO and BRVO trials differ in dosing regimen and trial duration as well as population differences, so the result of any indirect comparison would be subject to uncertainty. During the evaluation, the trials were reviewed. While the published articles omit variables regarding the study population, the inclusion criteria across the trials were fairly similar, and patient age was approximately the same across the trials. Trial duration was different, but the trials had multiple endpoints. This suggests that some comparisons across certain endpoints for some of the trials could be informative. In particular, an indirect comparison could be conducted using CRUISE and Epstein 2012 for CRVO. An indirect comparison for BRVO using BRAVO and Moradian 2011 would require conversion of the logarithmic BCVA results in Moradian as well as calculation of change from baseline so such a comparison may not be appropriate. The table below summarises available results for CRVO and BRVO trials and also provides the conclusions drawn by the authors of the papers.
|
Trial (active treatment arm) |
Outcome measure |
Mean (SD) bevacizumab/ ranibizumab |
Mean (SD) sham/ laser |
Results discussed in publication |
|---|---|---|---|---|
|
CRVO |
||||
|
CRUISE (ranibizumab) |
Change in BCVA from baseline at week 24 (95% CI) |
14.9 (12.6, 17.2) |
0.8 (-2.0, 3.6) |
Results taken from November 2013 resubmission |
|
Epstein 2012 (bevacizumab) |
Improvement in BCVA (number of letters) at week 24 |
14.1 (NA) |
-2.0 (NA) |
Intravitreal bevacizumab administered every 6 weeks for 6 months is superior to sham injection. After six months, all patients received intravitreal bevacizumab. |
|
Improvement in BCVA (number of letters) at week 48 |
16.1 (NA) |
4.6 (NA) |
||
|
BRVO |
||||
|
BRAVO (ranibizumab) |
Change in BCVA from baseline (95% CI) |
18.3 (16.0, 20.6) |
7.3 (5.1, 9.5) |
Results taken from November 2013 resubmission |
|
Russo 2009 (bevacizumab) |
Change in BCVA (logMAR) at 12 months |
0.31 (NA) |
0.2 (NA) |
Mean visual acuity and CMT improved at 1, 3, 6, and 12 months when treated with bevacizumab. According to authors, the use of bevacizumab for BRVO offers significant advantages over triamcinolone and grid-laser treatment. |
|
Change in CMT at 12 months |
416 (NA) |
273 (NA) |
||
|
Moradian 2011 (bevacizumab) |
Relative improvement in BCVA (LogMAR) at 12 weeks |
-0.31 (0.3) |
-0.15 (0.3) |
Improvements from baseline in BCVA for bevacizumab after 6 and 12 weeks were statistically significant. When comparing visual improvements between sham and bevacizumab groups, only visual improvements after 6 weeks were statistically different. After 12 weeks visual improvement in the two groups were not statistically different. |
|
Relative decrease (µm) in CMT at 12 weeks |
287.3 (167.8) |
59 (212.6) |
||
BCVA=best corrected visual acuity; CMT central macular thickness; GLP=grid laser photocoagulation; NA=not available; SD=standard deviation
Source: compiled during the evaluation
Comparative harms
6.11 The minor resubmission quoted the PBAC Minutes from November 2013 as follows: “The PBAC noted the results of the IVAN study which compared bevacizumab and ranibizumab in patients with age-related macular degeneration, found that fewer patients in the bevacizumab group experienced arteriothrombotic events or heart failure compared with the ranibizumab group (0.7% vs. 2.9%; OR=0.23; 95% CI: 0.05, 1.07; P=0.03)” (paragraph 6.9).
6.12 The minor resubmission contended that the CATT and IVAN trials actually revealed safety concerns for bevacizumab, and the pooled results of the two trials show that the pooled risks of deaths and serious events favour ranibizumab over bevacizumab, with the risk of arterial thrombotic events not favouring either treatment. The forest plot presented by the minor resubmission is reproduced below.
Pooled analysis of CATT and IVAN for adverse events
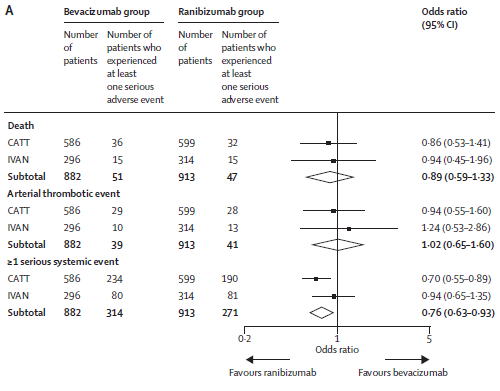
Source: Figure 1, pg 4 of the minor resubmission; taken from Chakravarthy et al (2013)
6.13 The minor resubmission presented no other safety data. For DME, the Nepomuceno 2013 trial provided little safety information. For RVO, a formal comparison of the safety outcomes of the included trials is not feasible given limited data available in the published papers. A summary of available safety conclusions for the evidence cited by the minor resubmission was collected during the evaluation and is shown in the table below.
|
Trial |
Key points regarding safety |
|---|---|
|
DME |
|
|
Nepomuceno et al 2013 |
No significant change in mean intraocular pressure at any study follow-up visit in either group. In the bevacizumab group, 1 patient experienced significant cataract progression and another developed transient vitreous haemorrhage after a vitreous detachment. 2 patients in the ranibizumab group developed endophthalmitis and 1 patient in the ranibizumab group experienced increased blood pressure and 1 patient developed transient worsening of renal function |
|
RVO |
|
|
CRUISE & BRAVO trials (safety conclusions from PBAC minutes) |
“The re-submission maintained that the overall incidence of adverse events is similar across treatment groups. The PBAC did not agree with the November 2012 submission’s claim, noting that in both trials there were more conjunctival haemorrhages (RD=12.6%; 95% CI: 0.6, 24.7) and retinal exudates (RD=10.9%; 95% CI: 1.4, 20.3) for ranibizumab compared with sham injections, with the differences being statistically significant in the BRAVO trial.” (paragraph 6.8, November 2013 PBAC Minutes) |
|
Epstein et al 2012 |
No endophthalmitis, retinal tear or retinal detachment during 24 week period. No serious non-ocular adverse events were reported. At week 24, 5 of the 30 sham patients developed iris rubeosis. The iris neovascularisation had regressed in all these patients by week 48 and no new cases of rubeosis were seen between weeks 24 and 48. |
|
Russo et al 2009 |
Injections were well tolerated in all patients. No cases of uveitis, endophthalmitis, ocular toxicity, or any obvious systemic adverse events were observed. No significant changes in intraocular pressure or lens status were observed during study follow-up. |
Source: compiled during the evaluation
Clinical claim
6.14 Overall, the minor resubmission presented weak evidence supporting a claim of equivalent effectiveness between ranibizumab and bevacizumab. As indicated above, no strong conclusion for comparative safety can be reached. The minor resubmission acknowledged this in its conclusion, where it states that the sponsor believes inadequate safety information exists to develop a comprehensive risk-benefit profile of bevacizumab against which ranibizumab could be assessed.
Economic analysis
6.15 The minor resubmission did not make any changes to the DME and RVO models presented in the November 2013 resubmissions. It presented model results using the requested prices in the November 2013 resubmission and a newly reduced requested price common to DME and RVO. The PBAC noted that the revised ICERs therefore differed across DME and RVO, however, they could not be relied upon as they retained same modelling approach, which inappropriately applied patient-based utilities to health states defined by the treated eye, which the PBAC has not accepted previously.
|
|
Ranibizumab |
Laser/sham injection |
Increment |
|---|---|---|---|
|
DME |
|||
|
November 2013 price (REDACTED) |
(REDACTED) |
(REDACTED) |
(REDACTED) |
|
New requested price (REDACTED) |
(REDACTED) |
(REDACTED) |
(REDACTED) |
|
QALYs |
(REDACTED) |
(REDACTED) |
(REDACTED) |
|
November 2013 ICER |
|
|
(REDACTED) |
|
Revised ICER |
|
|
(REDACTED) |
|
RVO |
|||
|
November 2013 price (REDACTED) |
(REDACTED) |
(REDACTED) |
(REDACTED) |
|
New requested price (REDACTED) |
(REDACTED) |
(REDACTED) |
(REDACTED) |
|
QALYs |
(REDACTED) |
(REDACTED) |
(REDACTED) |
|
November 2013 ICER |
|
|
(REDACTED) |
|
Revised ICER |
|
|
(REDACTED) |
Source: Table 6, pg 7 of the minor resubmission; revised RVO ICERs calculated during the evaluation.
Estimated PBS usage & financial implications
6.16 The submission’s estimates of what treatments would be used for DME, BRVO and CRVO in the absence of reimbursed ranibizumab are presented below.
|
Treatment |
DME |
BRVO |
CRVO |
|---|---|---|---|
|
Bevacizumab |
11% |
40% |
76% |
|
Laser |
50% |
22% |
0% |
|
Laser + bevacizumab |
33% |
28% |
0% |
|
Other |
7% |
10% |
24% |
Source: Table 5, pg 5 of the minor resubmission
6.17 The resubmission presents a summary of PBS/RPBS ranibizumab, aflibercept, and cancer-related bevacizumab claims as well as MBS claims for intravitreal injections for the 2012-13 financial year. These are summarised in the table below.
|
Scheme |
Ranibizumab |
Aflibercept |
Intravenous bevacizumaba |
|---|---|---|---|
|
PBS |
137,947 |
30,955 |
30,014 |
|
RPBS |
24,746 |
4,591 |
772 |
|
PBS/RPBS total |
162,693 |
35,546 |
30,786 |
|
Ranibizumab/aflibercept total |
198,239 |
|
|
|
MBS items |
Claims |
Unaccounted MBS claims |
|
|
42738 |
240,671 |
266,149 – 198,239 = 67,910 |
|
|
42739 |
9,281 |
||
|
42740 |
16,197 |
||
|
Total |
266,149 |
||
a These claims are for the PBS-listed cancer indications of intravenous bevacizumab, not intravitreal ocular injections.
Source: Tables 2 to 4 pg 5-6 of the minor resubmission and verified during the evaluation.
6.18 The minor resubmission suggested that the surplus of MBS claims for intravitreal injections, after ranibizumab and aflibercept claims are accounted for, reflects claims for off-label intravitreal bevacizumab.
7 PBAC Outcome
7.1 The PBAC considered that compounded bevacizumab was a relevant comparator because evidence of its current use in patients who would be eligible for PBS-subsidised ranibizumab. In the event of a PBS listing for ranibizumab for the treatment of DME and RVO, prescribers would replace compounded bevacizumab with ranibizumab.
7.2 The PBAC noted Departmental advice that, if compounded bevacizumab were to be considered for PBS listing, its pricing for PBS purposes would most likely reflect the approach to pricing already applied to bevacizumab as an oncology medicine through the Efficient Funding of Chemotherapy Program.
7.3 The PBAC considered that the presented evidence supported a claim of equivalent effectiveness, but the PBAC would prefer a more robust basis for assessing the comparative effectiveness and safety of ranibizumab and bevacizumab.
7.4 The PBAC considered that a comprehensive review of the comparative effectiveness and safety of ranibizumab and bevacizumab would be informative.
7.5 The PBAC noted that there are currently many trials either ongoing, or expected to begin enrolling in the near future, which would be applicable to this submission. The PBAC considered that these forthcoming trials may be of relevance and could provide a stronger evidence base.
7.6 The PBAC noted the price reduction offered in the submission, but also noted the previously identified issues with the utilities in the modelled economic evaluation had not been rectified in this resubmission. The PBAC did not consider the price reduction sufficient to offset its concerns regarding the economic model. Therefore the PBAC considered it appropriate to continue its deferral from November 2013.
Outcome:
Deferred
Context for Decision
The PBAC helps decide whether and, if so, how medicines should be subsidised in Australia. It considers submissions in this context. A PBAC decision not to recommend listing or not to recommend changing a listing does not represent a final PBAC view about the merits of the medicine. A company can resubmit to the PBAC or seek independent review of the PBAC decision.
Sponsor’s Comment
The intention of the submission was to formalise our objection that bevacizumab is a relevant comparator as well as dispute the PBAC claim that “in consideration of the current resubmission, the PBAC noted that numerous head-to-head studies comparing ranibizumab and bevacizumab have been conducted (Ratified Minutes – November 2013 PBAC Meeting). Novartis maintains the arguments presented in the submission against accepting bevacizumab as a comparator as indicated in section 5.3. The assertion of a ‘claim’ being made in the submission is incorrect, the purpose was to provide a summary of the evidence of lack of evidence, particularly regarding the safety of bevacizumab (section 6.5).



