Trastuzumab emtansine, injection, 100 mg and 160 mg, Kadcyla® - July 2013
Public Summary Document
Product: Trastuzumab emtansine, injection, 100 mg and 160 mg, Kadcyla®
Sponsor: Roche Products Pty Ltd
Date of PBAC Consideration: July 2013
1. Purpose of Application
The submission requested a Section 100 listing for trastuzumab emtansine (T-DM1) for treatmentof a patient with HER2-positive unresectable locally advanced or metastatic breast cancer who has received prior therapy with trastuzumab and a taxane and whose disease has progressed despite treatment with trastuzumab for metastatic disease, or within 6 months of completing adjuvant therapy.
This application was being processed under the TGA/PBAC parallel process. No TGA documents were available during the evaluation. A Clinical Evaluation report and a Delegate’s Overview proposing registration were available to the PBAC at the time of its meeting in July 2013.
Highly Specialised Drugs are medicines for the treatment of chronic conditions, which, because of their clinical use or other special features, are restricted to supply to public and private hospitals having access to appropriate specialist facilities.
2. Background
Trastuzumab emtansine had not previously been considered by PBAC.
Trastuzumab (rch) Herceptin® is currently available on the PBS for the treatment of:
- Locally advanced HER2 positive breast cancer
- Early HER2 positive breast cancer
3. Registration Status
Trastuzumab emtansine was TGA registered on 3 September 2013 as follow: KADCYLA, as a single agent, is indicated for the treatment of patients with HER2 positive metastatic (Stage IV) breast cancer who previously received trastuzumab and a taxane, separately or in combination. Patients should have either: received prior therapy for metastatic disease or, developed disease recurrence during or within six months of completing adjuvant therapy.
4. Listing Requested and PBAC’s View
Section 100 Efficient Funding of Chemotherapy (Public Hospital), and
Section 100 Efficient Funding of Chemotherapy (Private Hospital/Clinic)
Initial treatment
Initial treatment of patients with HER2-positive unresectable locally advanced or metastatic breast cancer (stage IV) who have received prior therapy with trastuzumab and a taxane and whose disease has progressed despite treatment with trastuzumab for metastatic disease or within 6 months of completing adjuvant therapy.
Authority applications for initial treatment of trastuzumab emtansine must be made in writing and must include:
(a) a completed authority prescription form
(b) a pathology report demonstrating HER2 positivity by in situ hybridization (ISH) or a score of 3+ by immunohistochemistry (IHC)
(c) date of last treatment with a taxane and total number of cycles
(d) a signed patient acknowledgment
(e) dates of treatment with trastuzumab and
(f) date of demonstration of progression whilst on treatment with trastuzumab.
Continuing treatment
Continuing treatment of patients with HER2-positive unresectable locally advanced or metastatic breast cancer (stage IV) who have previously received treatment with PBS subsidised trastuzumab emtansine and who do not have progressive disease.
Authority applications must be made in writing and must include:
(a) a completed authority prescription form and
(b) a statement from the prescribing doctor that the disease has not progressed.
Grandfather clause
Initial PBS-subsidised supply for continuing treatment with trastuzumab emtansine for a patient with:
1. HER2-positive unresectable locally advanced or metastatic breast cancer (stage IV)
2. Receiving treatment with trastuzumab emtansine prior to date of PBS listing
The PBAC noted that under the proposed restriction, patients whose breast cancer progresses more than six months after adjuvant therapy will need to use non-PBS trastuzumab (Herceptin®) and have their cancer progress further in order to qualify for treatment with trastuzumab emtansine.
The PBAC noted that the EMILIA trial specifically excluded patients who had previously received lapatinib plus capecitabine, and that there were therefore no data on the effectiveness of trastuzumab emtansine following lapatinib. The PBAC therefore considered that the PBS restrictions for trastuzumab emtansine and lapatinib should exclude the possibility of sequential use of an agent after failure of the other.
The PBAC noted that the proposed restriction did not specify the duration of previous treatment with trastuzumab. In the EMILIA trial, the median duration of prior trastuzumab treatment for patients receiving trastuzumab emtansine was 13.8 months (range 0 to149.8 months) and for patients randomised to lapatinib plus capecitabine was 13.9 months (range 0 to 115.9 months). The PBAC considered that these data suggested that the patient population had disease resistant to trastuzumab. The PBAC considered it difficult to determine how this could be specified in the PBS restriction.
The submission proposed a grandfather restriction for patients currently receiving trastuzumab emtansine outside the PBS. It will be possible for these patients to demonstrate HER2 status and provide prior treatment details and evidence of disease progression and therefore qualify under the proposed initial restriction. The PBAC did not consider that a grandfather restriction was required for initial treatment.
The PBAC considered that the PBS restriction should specify that treatment should not continue beyond disease progression.
The PBAC consider that the PBS restriction should specify only patients with Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, consistent with the key trial, EMILIA.
The submission proposed determination of HER-2 positive status either by in situ hybridization (ISH) or by a score of 3+ by immunohistochemistry (IHC). The PBAC considered that the PBS restriction should align with that for lapatinib which specifies that HER2 status must be demonstrated by ISH.
The PBAC noted that the prescribing requirements for the non-PBS Late Stage Metastatic Breast Cancer Program define HER-2 positive status differ from those for the current listing for lapatinib and that proposed for trastuzumab emtansine. The prescribing requirements for the non-PBS Late Stage Metastatic Breast Cancer Program are:
- An IHC score of 3+ or
- IHC 2+ with confirmation by ISH or
- Evidence by ISH.
The PBAC considered it appropriate to include a warning in the restriction for trastuzumab emtansine that use in patients with left ventricular ejection fraction (LVEF) less than 45% or with symptomatic heart failure is contraindicated, consistent with the PBS restriction for trastuzumab. A caution recommending standard cardiac function testing (echocardiogram or multigated acquisition (MUGA) scanning) prior to initiation and at regular intervals (e.g. every three months) during treatment was also considered appropriate.
5. Clinical Place for the Proposed Therapy
In Australia, trastuzumab has become the standard treatment for women with HER2 overexpressing breast cancer in the metastatic and early breast cancer setting. Overexpression of HER2 has been associated with poor prognosis and reduced overall survival.
While a proportion of patients diagnosed with HER2+ breast cancer who receive trastuzumab will no longer go on to develop more advanced forms of the disease, there continues to be a clinical need for additional treatment options for those patients whose disease progresses to metastatic breast cancer. Trastuzumab emtansine is a HER2-targeted antibody drug conjugate that contains the humanised anti-HER2 IgG1, trastuzumab, covalently linked to the microtubule inhibitory drug DM1.
The submission proposed that it will provide another treatment option for patients who need an additional treatment following trastuzumab.
6. Comparator
The submission proposed a mixed comparator:
- Lapatinib + capecitabine (40%)
- Trastuzumab + chemotherapy (58%)
- Trastuzumab monotherapy (2%).
The PBAC considered that lapatinib plus capecitabine was the appropriate comparator regimen, as the treatments most likely to be replaced in practice in patients with disease progression following trastuzumab for metastatic disease.
The PBAC noted that the submission estimated the proportions of comparators from a clinician survey (n=17), and the Ipsos database (n=24). The PBAC did not consider these data to be robust.
The PBAC noted that lapatinib + capecitabine may be displaced to third-line therapy following progression on trastuzumab emtansine rather than being replaced by trastuzumab emtansine as proposed in the submission.
7. Clinical Trials
The submission presented:
- one open-label head-to-head randomised controlled trial (RCT) comparing trastuzumab emtansine to lapatinib + capecitabine in 991 patients with locally advanced breast cancer (LABC)/metastatic breast cancer (MBC), or progressed within six months after completing adjuvant therapy (EMILIA);
- one open-label head-to-head RCT comparing trastuzumab emtansine to trastuzumab + docetaxel in 137 patients with LABC/MBC (4450);
- two supplementary open-label RCTs, used in an indirect comparison comparing:
- trastuzumab + capecitabine to capecitabine in 156 patients with LABC/MBC: GBG 26;
- lapatinib + capecitabine versus capecitabine alone in 408 patients with LABC/MBC: EGF100151;
- a meta-analysis of eight RCTs comparing HER2 agents (trastuzumab or lapatinib) to various chemotherapies in 1,848 patients with MBC (Harris (2010)); and
- ten non-randomised studies involving trastuzumab + chemotherapy in 511-627 patients with LABC/MBC.
These trials were used for two comparisons, one direct and one indirect, as shown in the table below:
|
|
|
Drug 1 |
Drug 2 |
Line of therapy |
|---|---|---|---|---|
|
Direct RCTs |
EMILIA |
Trastuzumab emtansine |
Lapatinib + capecitabine |
1st (fast-relapsing patients) + 2nd line |
|
4450 |
Trastuzumab emtansine |
Trastuzumab + docetaxel |
1st line |
|
|
Used in indirect comparison |
GBG 26 |
Trastuzumab + capecitabine |
Capecitabine |
1st (who had progressed following adjuvant therapy) + 2nd line |
|
EGF 100151 |
Lapatinib + capecitabine |
Capecitabine |
2nd line |
|
|
Harris (2010) |
Trastuzumab/ lapatinib + chemotherapy/ hormonal therapy |
Chemotherapy/ hormonal therapy |
1st + 2nd line |
|
|
non-randomised trials |
|
Trastuzumab |
Chemotherapy |
1st + 2nd line |
|
Section D & Section E |
|
Trastuzumab emtansine |
Lapatinib + capecitabine OR trastuzumab + chemotherapy OR trastuzumab monotherapy |
2nd line |
bid: twice daily, qd: once daily, q3w: once three weekly.
The table below details the published trials presented in the submission.
|
Trial ID/ First author |
Protocol title/ Publication title |
Publication citation |
|---|---|---|
|
EMILIA |
|
|
|
Verma S et al. |
Trastuzumab emtansine for HER2-positive advanced breast cancer. |
N Engl J Med 2012 Oct 1. DOI: 10.1056/NEJMoal1209124. |
|
Blackwell K. et al. |
Primary results from EMILIA, a phase III study of trastuzumab emtansine (T DM1) versus capecitabine (X) and lapatinib (L) in HER2-positive locally advanced or metastatic breast cancer (MBC) previously treated with trastuzumab (T) and a taxane. |
J Clin Oncol 2012 30: (Suppl; abstr LBA1). ASCO Annual Meeting, 2012.
|
|
Verma S.et al. |
EMILIA: A phase III, randomized, multicenter study of trastuzumab-DM1 (T-DM1) compared with lapatinib (L) plus capecitabine (X) in patients with HER2-positive locally advanced or metastatic breast cancer (MBC) and previously treated with a trastuzumab-based regimen. |
J Clin Oncol 2011;29 (suppl; abstr TPS116 ). ASCO Annual Meeting, 2011.
|
|
Verma S. et al. |
Updated overall survival results from EMILIA, a phase 3 study of trastuzumab emtansine (T-DM1) vs. capecitabine and lapatinib in HER2-positive locally advanced or metastatic breast cancer. |
Presentation at ESMO 2012 Congress; Vienna, Austria. |
|
Welslau M. et al. |
Patient-reported outcomes from EMILIA, a phase 3 study of trastuzumab emtansine (T-DM1) vs. capecitabine and lapatinib (XL) in HER2-positive locally advanced or MBC. |
Poster presentation 329P. ESMO 2012 Congress; Vienna, Austria. |
|
4450 |
|
|
|
Perez EA. et al. |
Efficacy and safety of trastuzumab-DM1 versus trastuzumab plus docetaxel in HER2-positive metastatic breast cancer patients with no prior chemotherapy for metastatic disease: preliminary results of a randomized, multicentre, open-label phase 2 study. |
Presentation at ESMO Annual meeting, 2010.
|
|
Hurvitz S. et al. |
Trastuzumab emtansine (T-DM1) vs trastuzumab plus docetaxel (H+T) in previouslyuntreated HER2-positive metastatic breast cancer (MBC): primary results of a randomized, multicenter, open-label phase II study (TDM4450g/B021976). |
Eur J Cancer 2011;47(Suppl. 330): Abstract 5001. |
|
Perez EA. et al. |
Efficacy and safety of trastuzumab-DM1 versus trastuzumab plus docetaxel in HER2-positive metastatic breast cancer patients with no prior chemotherapy for metastatic disease: Preliminary results of a randomized, multicenter, open-label phase 2 study (TDM4450G). |
Annals of Oncology 2010;21(Suppl. 8): viii2. Abstract LBA3.
|
|
Hurvitz SA. et al. |
Phase II randomized study of trastuzumab emtansine versus trastuzumab plus docetaxel in patients with human epidermal growth factor receptor 2–positive metastatic breast cancer. |
Published ahead of print on February 11, 2013 as 10.1200/JCO.2012.44.9694. The latest version is at http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.44.9694 |
8. Results of Trials
Direct comparison
For the direct comparison, the submission used EMILIA to demonstrate comparative effectiveness in patients treated as second line, and trial 4450 in first line treatment of advanced breast cancer patients.
The results of progression free survival and overall survival across the direct randomised trials are presented in the following table:
|
Trial ID |
Trastuzumab emtansine Median months (95% CI) |
Comparator* Median months (95% CI) |
Absolute Difference |
HR (95% CI)# |
|---|---|---|---|---|
|
Progression free survival |
|
|
|
|
|
EMILIA (IRC assessed) as at 14 January 2012 |
9.6 (N=495) |
6.4 (N=496) |
3.2 |
0.65 (0.59, 0.77) P<0.0001 |
|
4450 (investigator assessed) |
14.2 (N=67) |
9.2 (N=70) |
5.0 |
0.59 (0.36, 0.97) P=0.0353 |
|
Overall survival |
|
|
|
|
|
EMILIA as at 14 January 2012 |
NE (N=495) |
23.3 (N=496) |
NE |
0.62 (0.48, 0.81) P=0.0005 |
|
EMILIA as at 31 July 2012 |
30.9 (N=495) |
25.1 (N=496) |
5.8 |
0.68 (0.55, 0.85) P=0.0006 |
|
4450 |
NE (N=67) |
NE (N=70) |
NE |
1.059 (0.477, 2.352) P=0.8885 |
*Lapatinib + capecitabine in EMILIA and trastuzumab + docetaxel in 4450. #stratified analysis. IRC: independent review committee; HR: hazard rate ratio; N: number of patients; NE: not evaluable.
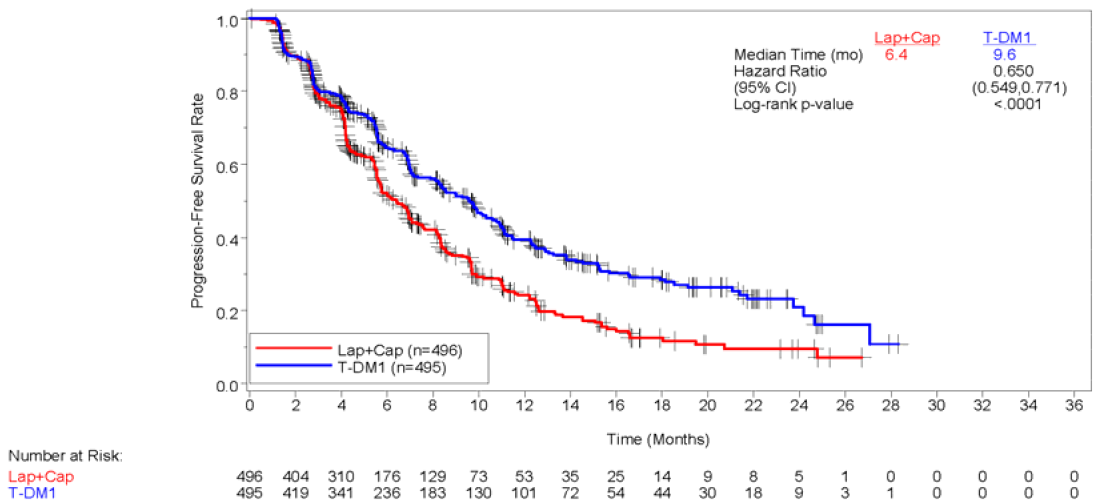
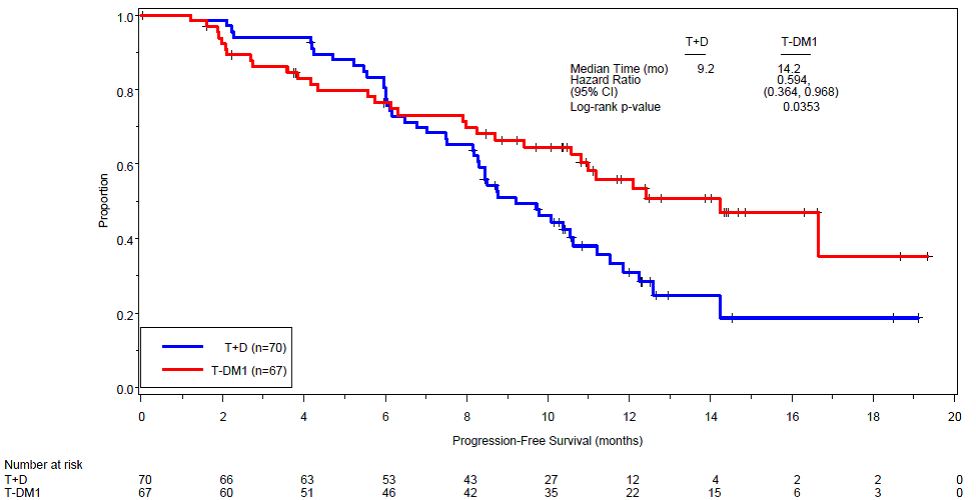
The trials showed that treatment with trastuzumab emtansine resulted in a significant increase in PFS in both EMILIA and 4450. Sub-group analysis based on results from EMILIA found that PFS gains (assessed by the trial’s independent review committee) were smaller in patients with the following characteristics:
- aged 65 years or older (HR=1.06, 95%CI: 0.68, 1.66);
- with non-visceral disease involvement (HR=0.96, 95%CI: 0.71, 1.30);
- with worse ECOG performance status (HR=0.76, 95%CI: 0.59, 0.98); and
- with non-measureable disease at baseline (HR=0.91, 95%CI: 0.59, 1.42).
Patients who had not received prior systemic therapy for MBC (HR=0.51, 95%CI: 0.30, 0.85) (i.e. fast-relapsing patients) benefited slightly more than those who had received prior systemic therapy for MBC the (HR=0.69, 95%CI: 0.58, 0.82), although the difference was not statistically significant.
The submission also presented estimates of objective response rate (ORR), clinical benefit rate (CBR), and investigator-assessed progression-free survival (PFS). Also presented for EMILIA were duration of response, TTF, and time to symptom progression:
- IRC- and investigator-assessed ORR was significantly larger with trastuzumab emtansine in EMILIA. Investigator-assessed ORR was larger, but not statistically significant, in 4450. In EMILIA and 4450 most patients treated with trastuzumab emtansine experienced a partial response rather than a complete response.
- Investigator-assessed PFS and TTF were statistically significantly larger with trastuzumab emtansine in EMILIA.
- Duration of response was longer (statistical significance not tested) in EMILIA and 4450.
- Time to symptom progression was significantly longer with trastuzumab emtansine in EMILIA and 4450: In EMILIA: median 7.1 months for trastuzumab emtansine, compared to 4.6 months for lapatinib+capecitabine (HR = 0.796, 95% CI = 0.667, 0.951; p=0.0121); in 4450: median 7.5 months for trastuzumab emtansine compared to 3.5 months for trastuzumab + docetaxel arm.
The PBAC agreed that confounding (by disease severity and prior treatment regimens) was a likely issue in trial 4450. In trial 4450 fast relapsing patients could not be identified. Approximately 23% of patients in 4450 had received prior trastuzumab and therefore may potentially meet the definition of “fast relapsers” following adjuvant trastuzumab. The PBAC noted the submission’s claim that the proportion of these fast-relapsing patients in patients to be treated is low (approximately 12% in the EMILIA trial). The PBAC considered that the effect size in the EMILIA trial may not be seen in the Australian population as the proportion of fast relapsing patients and stage IV patients enrolled in EMILIA was greater than in the Australian context.
The PBAC noted that treatment with trastuzumab emtansine resulted in a significant increase in PFS in both the EMILIA and 4450 trials.
The Kaplan-Meier plot of IRC-assessed PFS in the EMILIA trial (14 January 2012) is shown in the following figure:
The Kaplan-Meier plot of investigator-assessed PFS in 4450 (November 2010 data) is shown in the following figure:
The PBAC noted also a statistically significant increase in OS of 5.8 months over lapatinib plus capecitabine in the EMILIA trial. The PBAC noted also that no OS benefit was observed in the 4450 trial.
The Kaplan-Meier plot of OS in the EMILIA trial (31 July 2012) is shown in the following figure:
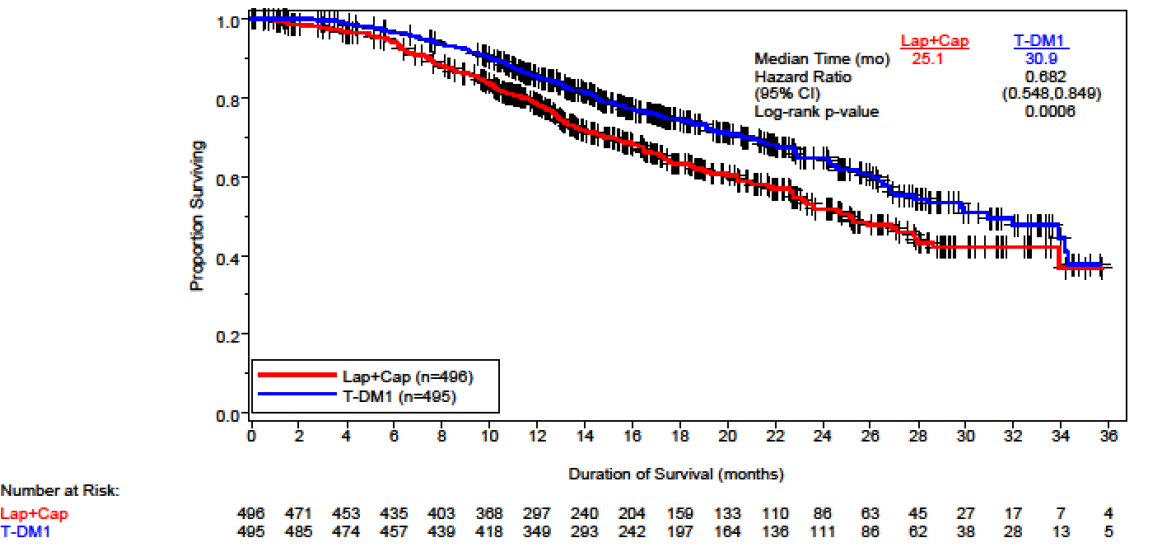
The PBAC noted that the 4450 trial had potential confounding in that fewer patients had died, there was a high rate of crossover and high numbers of patients received at least one non-protocol treatment.
The PBAC noted subgroup analyses of EMILIA that showed similar differences to PFS, albeit these differences were not statistically significant.
Indirect comparison
The submission presented a two-step indirect analysis between trastuzumab emtansine and trastuzumab plus chemotherapy to justify the use of lapatinib plus chemotherapy in the base case of the economic evaluation.
- Step one compares trastuzumab plus chemotherapy via trastuzumab plus docetaxel with lapatinib plus capecitabine.
- Step two compares trastuzumab plus chemotherapy and trastuzumab emtansine via the common reference of lapatinib plus capecitabine from the EMILIA trial to establish the magnitude of the claimed incremental benefit of trastuzumab emtansine over trastuzumab plus chemotherapy. These results informed the sensitivity analysis and the economic evaluation.
The PBAC noted the following:
- In the first indirect comparison, there is a trend towards lapatinib + capecitabine showing superiority over trastuzumab + capecitabine in second line.
- Due to cross-over in GBG 26 and EGF100151, the second indirect comparison OS results favour trastuzumab emtansine. Overall, the second indirect comparison results are more favourable towards trastuzumab emtansine compared to the results of 4450.
The PBAC considered that the claim that trastuzumab + capecitabine is interchangeable with trastuzumab + chemotherapy was not adequately supported, particularly as the Harris (2010) meta-analysis includes eight RCTs which differ in the following ways:
- The method of determining HER2 status
- The line of therapy
- The amount of cross-over (5 of the 8 trials)
- The duration of follow-up
- The treatments given to patients in terms of combining trastuzumab and lapatinib together, and a variety of chemotherapies or hormonal therapies at different doses and durations.
- Whether and how the trials were blinded
- The methods of analysis.
The PBAC noted that only two trials enrolled patients for second-line therapy were GBG 26 and EGF100151, which were already included in the indirect comparison.
The PBAC considered that although the results from the indirect analysis favour trastuzumab emtansine, the confidence intervals are wide and include the null.
With regard to comparative harms, in EMILIA, trastuzumab emtansine was associated with more cases of hepatotoxicity, thrombocytopenia/bleeding, and infusion reactions but fewer cases of gastrointestinal toxicity, mucosal inflammation and hand-foot syndrome compared to lapatinib + capecitabine. In terms of treatment related grade 3 or greater adverse events (AEs), trastuzumab emtansine was associated with statistically significantly more cases of hepatotoxicity and thrombocytopenia.
In trial 4450 trastuzumab emtansine was associated with more cases of hepatotoxicity, headache, and infusion reactions, but fewer cases of neutropenia, alopecia, gastrointestinal toxicity, and peripheral oedema. In terms of treatment related grade 3 or greater AEs, trastuzumab emtansine was associated with statistically significantly more cases of hepatotoxicity and pneumonia
In EMILIA, the overall incidence of cardiac dysfunction and decreases in LVEF was low. In 4450 the overall incidence of cardiac dysfunction and decreases in LVEF was higher compared to EMILIA, but incidence was higher with trastuzumab + docetaxel compared to trastuzumab emtansine (and lower than was seen in previous RCTs involving trastuzumab). EMILIA and 4450 did not enrol patients with LVEF less than 50% or patients with a history of CHF, history of myocardial infarction, unstable angina or serious cardiac arrhythmia.
9. Clinical Claim
The submission described trastuzumab emtansine as superior in terms of comparative effectiveness and superior in terms of comparative safety over lapatinib + capecitabine.
The PBAC considered that, based on the results of the EMILIA trial, this claim was adequately supported.
The submission also described trastuzumab emtansine as superior in terms of comparative effectiveness and superior in terms of comparative safety over trastuzumab + chemotherapy.
The PBAC considered that this was not well supported as it was based on the claim that trastuzumab plus capecitabine is equivalent in efficacy to trastuzumab with any other chemotherapy. The PBAC considered that although the results from the indirect analysis favour trastuzumab emtansine, the confidence intervals are wide and include the null.
10. Economic Analysis
The submission presented a modelled economic evaluation (CUA) based on the claim of superior efficacy and safety. The weighted ICER was $45,000 - $75,000/QALY, constructed by weighting the base case ICER against lapatinib+capecitabine of $75,000 - $105,000/QALY and the base case ICER against trastuzumab+chemotherapy of $15,000 - $45,000/QALY. The proportion of patients in each health state was based on PFS and OS from EMILIA, applied to patients with LABC and MBC (second-line therapy) and extrapolated to seven years duration (from 12.39 months in the trial) and applying utility weights from Lloyd (2006).
An ‘Area under the curve (AUC)’ model was used to evaluate cost-effectiveness. Patients are assumed to be in one of three mutually exclusive health states:
- PFS (within which patients may be responders/non-responders)
- Progressive disease (PD), and
- Death.
Three treatment options are considered:
- trastuzumab emtansine
- Lapatinib + capecitabine, and
- Trastuzumab-based treatments (trastuzumab + chemotherapy and trastuzumab monotherapy).
The proportion of patients in each health state is based on the Kaplan-Meier estimates for PFS and OS in EMILIA, or fitted survival functions (using a gamma distribution). The Kaplan-Meier estimates are used up to 12.39 months, which is then extrapolated to a seven year time horizon as the base case. The PBAC considered the model structure reasonable.
The PBAC noted the following issues with the model’s assumptions:
- The same efficacy and incidence of adverse events (except alopecia) was assumed for trastuzumab+chemotherapy as for lapatinib+capecitabine. The PBAC noted the different safety profiles of the two regimens and did not consider that this assumption was appropriate.
- Disutilities applied to AEs were assumed ongoing. The PBAC considered that this may not be appropriate for all AEs (e.g. diarrhoea & vomiting).
- No treatment costs were assumed post-progression. The PBAC noted that this approach favoured trastuzumab emtansine, as survival is longer in that arm of the model.
- Post progression utilities were assumed to be the same for all treatments.
The PBAC noted the following issues in applying the trial results to the PBS population:
- The applicability of the comparator arm in the EMILIA trial as a proxy for trastuzumab+chemotherapy (the other therapy likely to be replaced) was based on the indirect comparison presented in clinical evidence. As the indirect comparison was not considered to be reliable, this affected the applicability of the results to the PBS population.
- Patient characteristics were assumed to be similar, but the estimates of age and weight were based on IPSOS data which had a small sample size for this patient population (n=24);
- There were more Stage IV and fast relapsing patients in EMILIA than likely to be in the Australian population.
The PBAC noted the following issues with the submission’s extrapolation of the trial results:
- Kaplan-Meier estimates for Time To Off Treatment (TTOT) from EMILIA were used until the pooled median follow-up (at first cut-off). The PBAC noted that the use of the HR at first cut-off (0.68) rather than the second cut off (0.62) favoured trastuzumab emtansine.
- The use of TTOT rather than PFS accounts for discontinuations, but assumes longer time on treatment for lapatinib+capecitabine than with PFS, thereby favouring trastuzumab emtansine.
Extrapolated survival curves based on a gamma distribution were fitted to PFS and OS, and used to model the transition probabilities. The PBAC considered that the choice of gamma distribution was reasonable, but noted the sensitivity of the ICER to the extrapolation of OS. The PBAC considered the seven year follow up was reasonable based on literature, but noted most of the data is extrapolated. The PBAC considered that the effect of a five-year time horizon on the ICER would be informative.
The utilities were based on a paper by Lloyd (2006) which estimates utilities for metastatic breast cancer states using hypothetical scenarios via a standard gamble task in a sample drawn from the UK general population (N=100). The submission then used a mixed model analysis to generate estimated coefficients to calculate disutilities.
The PBAC considered that how age was factored into the model was not transparent, noting that Lloyd et al included the age of the valuation respondent, not the person in the hypothetical scenario.
The model did not include disutilities for thrombocytopenia, neutropenia and elevated liver enzymes. The submission noted that there was no literature to suggest specific disutility for these adverse events. The PBAC noted that the omission of these adverse events, noting that trastuzumab emtansine was associated with statistically higher rates of these events compared with lapatinib+capecitabine.
The PBAC noted that the utilities in Lloyd et al relate to first line treatment but were treated in the model as applying to second line treatment.
The model applied a utility for progression of 0.55 in model, which the submission argued was conservative. The PBAC did not agree this was conservative, noting that as patients on trastuzumab emtansine spend less time in this state this approach favours trastuzumab emtansine.
The PBAC noted that with the submission’s estimates of costs and resource use was based largely on a survey of 17 oncologists. The PBAC considered that the majority of the assumptions were reasonable or conservative (favouring the comparator), except:
- No treatment costs were assumed post-progression.
- The extent of cost-offsets from substitution away from trastuzumab.
- The use of TTOT Kaplan-Meier estimates for length of treatment, favouring trastuzumab emtansine
The base case ICER for trastuzumab emtansine vs. lapatinib+capecitabine (second line treatment) was between $75,000 - $105,000 and vs. trastuzumab+chemotherapy (first line treatment) was between $15,000 - $ 45,000. Overall, the submission claimed a combined weighted ICER of $45,000 - $75,000.
Overall, the PBAC noted that the model is most sensitive to:
- The weighting of the ICER between the base case ICER against lapatinib+capecitabine ($75,000 - $105,000) and against trastuzumab+chemotherapy ($15,000 - $45,000). The PBAC noted that the higher the proportion of weighting of lapatinib+capecitabine, the higher the ICER.
- The time horizon of the model - ICER $45,000 - $75,000 for a 5 year time horizon
- Extrapolation of OS - ICER $45,000 - $75,000 using survival curves of trastuzumab + chemotherapy based on the indirect comparison: PFS HR = 0.52, OS HR = 0.59)
- Utilities - ICER $75,000 - $105,000 when treating utilities from Lloyd (2006) as first-line utilities (thus in the model all have already experienced disease progression, and then receive another disutility following 2nd progression)
11. Estimated PBS Usage and Financial Implications
The submission estimated a net cost per year to the PBS of $10 – $30 million in Year 5.
The submission proposed a rebate on Commonwealth PBS expenditure for trastuzumab emtansine.
12. Recommendation and Reasons
The PBAC rejected the submission on the basis of incorrect comparator. The PBAC considered that the correct comparator is lapatinib+capecitabine, and noted that the ICER against this regimen is unacceptably high.
The PBAC noted that the ICER was dependent on unjustified assumptions regarding the clinical management algorithm, particularly the extent of replacement of lapatinib+capecitabine.
The PBAC acknowledged the clinical need for new treatment for patients with HER2 positive breast cancer whose disease is no longer sensitive to trastuzumab. The PBAC noted and acknowledged the consumer comments from both patients and organisations that trastuzumab emtansine is viewed as presenting a treatment option after Herceptin for metastatic disease. The PBAC acknowledged the clinical need for other treatment options for metastatic breast cancer, and noted rapidly evolving treatment algorithms for this disease.
The PBAC considered that the mixed comparator was not appropriate, and that lapatinib+capecitabine would be the therapy most likely replaced. The PBAC noted that at the price proposed, trastuzumab emtansine is not cost effective against lapatinib+capecitabine. The inclusion of trastuzumab+chemotherapy as a comparator reduces the ICER to a level which, although superficially acceptable, is not a true reflection of trastuzumab emtansine’s cost effectiveness.
The PBAC noted also the possibility that rather than being replaced by trastuzumab emtansine, lapatinib+capecitabine will be displaced to third line treatment, thereby increasing the cost to the Commonwealth. The PBAC considered that use of lapatinib after failure of trastuzumab emtansine should be excluded by any future PBS restriction.
The PBAC considered the model structure to be reasonable but noted a number of assumptions that inappropriately favour trastuzumab emtansine, including omission of adverse events for which trastuzumab emtansine has a higher incidence, no post-progression treatment costs and all adverse events assumed to be ongoing.
The PBAC considered that the evaluation of trastuzumab emtansine would need to take account of treatment scenarios/algorithms according to whether the disease is sensitive or insensitive to trastuzumab either used as monotherapy or in combination with cytotoxic chemotherapy.
The PBAC considered that the patient population in the 4450 trial is different to the intended patient population. The 4450 trial population had treatment sensitive disease, and therefore is not relevant to this to this submission. The PBAC considered that the EMILIA trial should form the basis for the submission’s claims.
The PBAC noted the sensitivity of the model to the seven year time horizon, and considered a resubmission should include a five year time horizon as the base case.
The PBAC considered that a substantial price reduction would be required to achieve an acceptable ICER in the context of the comparator being 100% lapatinib+capecitabine.
The PBAC resolved to advise the Minister that in addition to the issues previously noted with the non-PBS Herceptin Program, another consequence of the Program is that it continues to set a pricing benchmark for the treatment of HER2 positive metastatic breast cancer which support cost ineffective treatment.
Outcome:
Rejected
13. Context for Decision
The PBAC helps decide whether and, if so, how medicines should be subsidised in Australia. It considers submissions in this context. A PBAC decision not to recommend listing or not to recommend changing a listing does not represent a final PBAC view about the merits of the medicine. A company can resubmit to the PBAC or seek independent review of the PBAC decision.
14. Sponsor’s Comment
The PBAC accepted that there is a clinical need for new treatment for patients with HER2 positive breast cancer whose disease is no longer sensitive to trastuzumab. Roche is committed to addressing the outstanding issues of concern in a resubmission to the earliest available PBAC meeting.




